Implementing Physical Activity Recommendations in Clinical Practice: A Survey of Oncology Nurses’ Perspectives
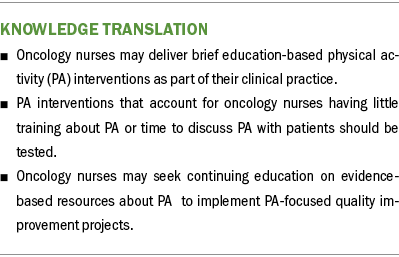
Problem Statement: Better understanding of oncology nurses’ perspectives about how interventions should be designed can promote physical activity (PA) in clinical settings.
Design: 75 oncology nurses completed online surveys.
Data Sources: A published survey, guided by the Consolidated Framework for Implementation Research, was used to assess multilevel factors that influence implementation of evidence-based interventions.
Analysis: Descriptive statistics were applied to quantitative data; directed content analyses were applied to qualitative data.
Findings: Participants believed it was important to discuss PA with patients; however, they had limited self-efficacy and resources to provide PA counseling. Barriers to providing counseling included competing clinical demands and a lack of education about PA for cancer survivors and resources.
Implications for Practice: Findings inform how interventions can be designed for implementation and sustained practice change in clinical settings. Integration of PA education in routine clinical practice will lead to increased PA and, ultimately, improved quality of life among cancer survivors.
Jump to a section
Physical activity (PA) promotion has always been part of oncology nursing. The field of exercise oncology was initiated by nurses who, countering beliefs about patients needing to rest and avoid activity during cancer treatment, were the first to test an exercise intervention and discovered that exercise may decrease chemotherapy-induced nausea (Jones & Alfano, 2013; MacVicar et al., 1989; Winningham et al., 1989; Winningham & MacVicar, 1988). Despite widely agreed on PA guidelines and decades of evidence that PA improves cancer outcomes, few people living beyond a cancer diagnosis engage in PA as recommended (Campbell et al., 2019; Patel et al., 2019; Schmitz et al., 2019). Nurses play a critical role in leading practice changes to better support patients’ engagement in PA as recommended.
PA is recognized as an important aspect of cancer care that is safe for patients on active treatment and for those who have completed treatment, regardless of cancer type (Campbell et al., 2019; Rock et al., 2022). For people living past a cancer diagnosis, guidelines are available from the American Cancer Society and the American College of Sports Medicine (ACSM) to ensure the maximum benefit can be gained. These guidelines include recommendations for 150–300 minutes of moderate activity per week, 75–150 minutes of vigorous activity per week, or a combination of moderate and vigorous activity, combined with muscle-strengthening activities two times per week (Campbell et al., 2019; Rock et al., 2022). PA benefits the physical, mental, and emotional health of people living past a cancer diagnosis (Turner et al., 2018). These benefits can include a reduction in mortality, the recurrence of some cancers, and the side effects/symptoms of cancer and cancer treatment (e.g., fatigue, pain, sleep), as well as improved quality of life, physical function, and mental and emotional well-being (Rock et al., 2022; Turner et al., 2018).
Despite documentation of PA’s beneficial effects, people living past a cancer diagnosis continue to have low levels of PA participation. A cross-sectional study of people living past a cancer diagnosis indicated that 93% of the study population was not active at levels recommended by ACSM (Avancini et al., 2020). These low participation levels indicate that decades of evidence supporting the benefits of PA for survivors of cancer and accepted national recommendations are insufficient to promote PA in this population. There is a pressing need to understand how patients living beyond a cancer diagnosis may be better supported to achieve evidence-based PA recommendations.
Multiple evidence-based PA interventions exist, but numerous barriers affect their delivery. Although clinicians have the unique ability to influence patient lifestyle and health behaviors—including PA education and promotion (Alderman et al., 2020)—no clear policy or practice establishes which member of the clinical team should provide PA education to people living beyond a cancer diagnosis. This lack of clarity creates a clinical gap, leaving the ownership of PA education within the oncology setting without a specific champion. Oncology nurses are ideally suited to meet this need by initiating early and continuous conversations about PA and providing patients with PA resources (Keogh et al., 2017). Compared to other members of the oncology care team, nurses have more frequent communication with patients; this creates strong nurse–patient relationships that significantly influence patients’ experiences and outcomes (Prip et al., 2018). In addition, because nurses are the most trusted professionals in the United States (Saad, 2022), the education they provide is likely to be effective. Findings from a systematic review indicate that patients want to receive PA counseling through cancer treatment centers from cancer-specific fitness experts or clinicians, including nurses (Wong et al., 2018). Oncology nurses can lead the way in promoting PA among patients by providing critically needed education and introducing patients to options for incorporating PA into their treatment plan.
Prior research has indicated that oncology nurses should assess patients’ current PA, review established evidence-based PA recommendations with patients, and link patients with resources to support engagement in PA (Bernardo & Becker, 2016; Rock et al., 2022; Schmitz et al., 2019). However, the literature has identified barriers to oncology nurses providing such PA education, including limited knowledge about PA recommendations and a lack of PA resources to share with patients (Alderman et al., 2020; Cantwell et al., 2018; Hardcastle et al., 2018; Nadler et al., 2017). Thus, for oncology nurses to provide PA education, interventions that consider nurses’ clinical demands and perspectives are needed. A systematic and comprehensive understanding of the factors that affect nurses’ provision of PA can lead to the development of PA interventions that are feasible to implement and sustain as part of nursing practice.
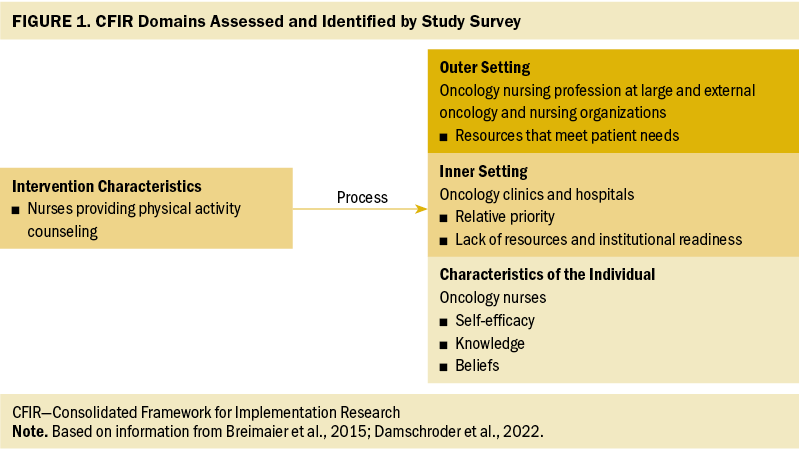
The current study sought to provide an in-depth understanding of oncology nurses’ provision of PA education by drawing on the principles of implementation science. Implementation science seeks to understand the factors that affect the adoption and maintenance of evidence-based practices into clinical settings (National Institutes of Health, 2016). The 2019–2022 Oncology Nursing Society (ONS) Research Agenda advises the use of implementation frameworks to improve translation of research into clinical practice (Von Ah et al., 2019). One such framework is the Consolidated Framework for Implementation Research (CFIR), which describes levels (i.e., intervention, outer setting, inner setting, and individual level) that influence implementation (Breimaier et al., 2015; Damschroder et al., 2009, 2022; Leeman et al., 2019). In this study, the CFIR was used to organize oncology nurses’ perspectives on the barriers and facilitators to providing PA recommendations to patients. The purpose of this study was to inform the development of a nurse-led PA intervention that considers implementation factors at the time of its design. The results from this study will lay the groundwork for future interventions by identifying nurses’ perspectives on multilevel factors that influence the uptake of evidence-based PA interventions in clinical practice.
Methods
Oncology nurses were surveyed between March and May 2020. Eligibility criteria included having an RN license and at least six months of experience caring for patients with cancer within the past year. Because this implementation research study aimed to understand the multilevel factors that influence implementation in the oncology setting, target enrollment was set at 100 to meet the laws of normal data distribution and provide a range of responses. To account for participant burden and the COVID-19 pandemic, the research team shared study information on their local ONS chapter’s page on Facebook to assess interest in participation. This decision was made based on consultation with the chapter leadership and the research team’s personal experiences during the pandemic.
Following a convenience sampling approach, Facebook postings were used to recruit participants. The study’s page on Facebook linked potential participants to a secure REDCap (Harris et al., 2009) study screening, consent, and survey completion site. Participants who completed the survey were mailed a $30 gift card.
The survey included a questionnaire that is published elsewhere (Hirschey, Nance, et al., 2021); it contained 7 open-ended and 26 closed-ended questions. The research team designed the questionnaire to elicit oncology nurses’ perspectives on the multilevel factors that influence implementation of PA recommendations in clinical practice (Younas & Porr, 2018) (see Figure 1). Prior to administration, the questionnaire was refined through two rounds of cognitive interviewing with oncology nurses, during which a think-aloud process was used to establish the validity of survey questions. This cross-sectional study was approved by the University of North Carolina Institutional Review Board.
Analyses
Descriptive statistics were conducted in R, version 4.1, to describe the study sample and analyze quantitative data. Directed content analysis was applied to qualitative data from the open-ended questions (Hsieh & Shannon, 2005). Specifically, the CFIR domains were used as coding categories to group participant responses as they related to (a) characteristics of individuals (e.g., self-efficacy, knowledge, beliefs of the individuals implementing the intervention); (b) characteristics of the inner setting (e.g., relative priority, resources, readiness for implementation); (c) characteristics of the outer setting (e.g., policies, organizations meeting patient needs); or (d) characteristics of the interventions (e.g., feasibility and adaptability of the intervention, evidence). All codes were applied by one researcher (M.W.) and reviewed through discussion with a second researcher (R.H.).
Results
Participant Demographics
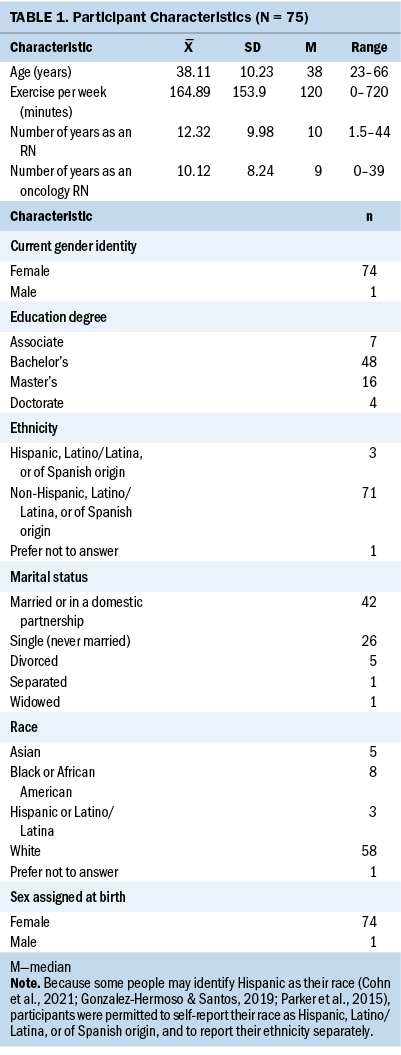
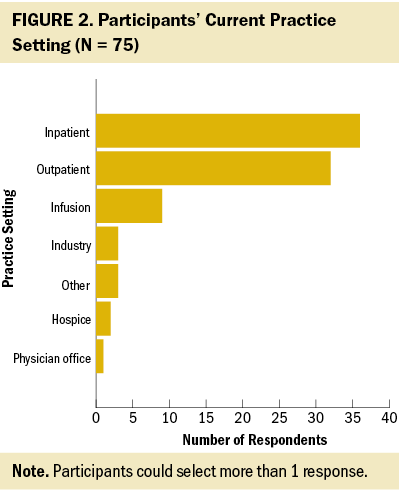
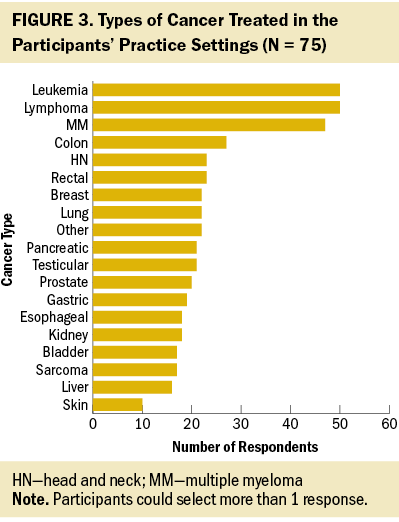
A total of 109 nurses completed the screening process. Of those, 105 nurses were eligible for the survey, and 77 provided online informed consent. Seventy-five participants completed the survey. Responses to open-ended questions ranged from 1 to 78 words in length, with an average of 17 (SD = 6) words. Most participants were non-Hispanic, White, cisgender, and female, and held a bachelor’s degree (see Table 1). About one-third of participants were oncology certified. Participants worked in a variety of clinical oncology settings (see Figure 2) and cared for patients living beyond a wide range of cancer diagnoses (see Figure 3). Survey findings are organized by CFIR domain (i.e., characteristics of the individual, inner setting, outer setting, and intervention characteristics) and detailed in the following sections.
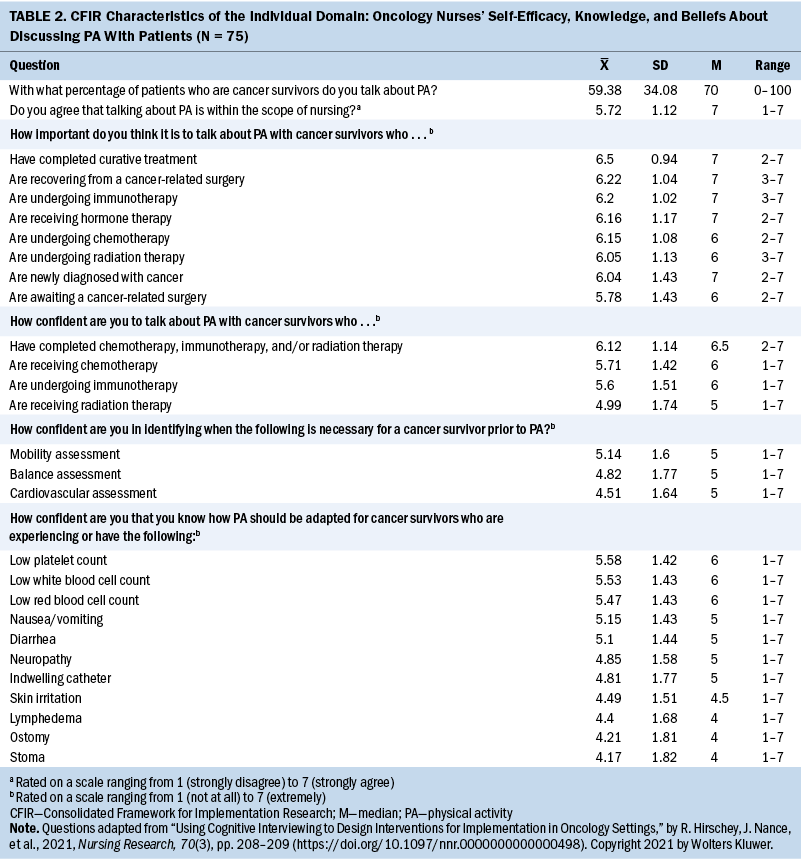
CFIR Characteristics of the Individual Domain: Oncology Nurses
Self-efficacy, knowledge, and beliefs: Several characteristics of oncology nurses were identified that influence how they provide PA recommendations to patients. Participants reported that they talk about PA with a mean of 59.38 (SD = 34) patients. As detailed in Table 2, quantitative data revealed that participants believe it is important to talk about PA with all patients, but they did not have high self-efficacy about their ability to do so. Many participants were not aware of the American Cancer Society or ACSM PA guidelines. When the published guidelines were listed at the conclusion of the survey, several participants left open-ended comments, such as “I did not know these recommendations existed” and “I wasn’t aware of these recommendations, but I enjoyed learning about them.” In summary, the most common responses about why oncology nurses were not talking about PA were related to feelings of unpreparedness and lack of knowledge.
Among participants, various personal beliefs were held about the appropriateness of talking about PA with patients. Participants shared that they do not talk about PA with all patients because “some patients are very sick, recovering from surgery, have activity restrictions, can’t leave their room, [or] have restrictions of going into public” and nurses are “not wanting to overwhelm patients in circumstances that are already overwhelming.” Another participant explained, “When patients are diagnosed, the focus tends to be on pharmacological treatment plans, coping, and emotional/physiological strength to tolerate [the] treatment plan,” and there is so much information for patients to process. However, participants shared that despite these challenges, they prioritize PA promotion and believe “it should be as high of a priority as taking medications appropriately because PA can drastically affect how well patients respond to treatment.” In addition, one participant said that they have “taken personal initiative to work PA recommendations into the personal care [they] provide because [they] have seen the benefits for patients.” These results indicate there is a range in nurses’ beliefs about whether they should recommend PA to patients, particularly those newly diagnosed with cancer.
CFIR Inner Setting Domain: Oncology Clinics and Hospitals
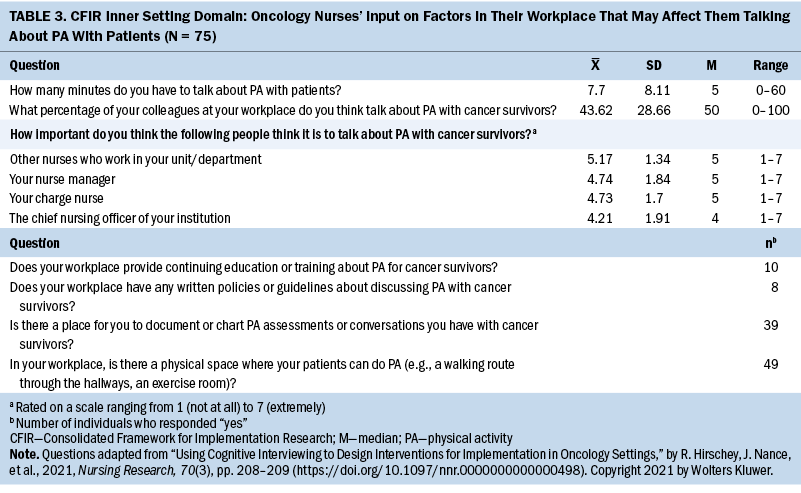
Quantitative data revealed that oncology nurses have little time—on average less than eight minutes—to talk about PA with patients and that they believe less than half (mean = 43.62) of their nurse colleagues talk about PA with patients (see Table 3). In addition, few resources were identified in participants’ workplaces to support them in providing PA recommendations. Only 10 participants indicated they are offered continuing education on the topic, and 39 indicated that there is not a place for them to chart their PA assessments and patient education.
Findings from qualitative data identified several workplace barriers that impede oncology nurses from providing PA counseling in the outpatient setting, as well as facilitators to providing PA counseling in outpatient and inpatient settings. These barriers are detailed in the following sections.
Relative priority: Participants identified a lack of time as the biggest barrier in their workplace for them to talk about PA with patients. They explained that they have limited time with patients and need to prioritize accordingly. For example, one participant said, “It can be difficult at times to focus on PA when nurses have so many tasks at hand to accomplish in a shift. PA can be pushed to the side if a patient is really sick and requires a lot of medical intervention.”
Similarly, another participant expressed, “In [the] outpatient infusion center, time is so limited because of patient load and emphasis on finishing treatment and getting another patient for treatment.” Overall, oncology nurses indicated that they simply do not have enough time with patients to assess PA and provide PA recommendations.
Lack of resources and institutional readiness: Results also revealed that many oncology care settings do not provide standard resources and procedures to support nurses in talking about PA with patients. One participant stated, “It’s never really been addressed, such as during orientation and training for the oncology unit. Therefore, nurses don’t feel comfortable discussing it, or [know] how to suggest PA to patients with a specific condition.” Of the 75 participants, only 12 identified PA resources at their workplace, including “inpatient exercise programs,” “discharge instructions,” “survivorship clinic,” “nurse educator plans activities for staff,” “telehealth lectures,” and “lunch-and-learn activities.” Only eight participants identified institutional policies that support nurses in promoting PA, which consisted of “inclusion in patient education materials or handbooks” and “access to the intranet.” When provided an open-ended text field to indicate where nurses may chart PA assessments or education, a variety of places were listed, including “nurses note,” “education tab,” “care plan,” “daily care activity flowsheet,” “discharge paperwork,” “activity assessment,” “rounding section of chart,” “whiteboard,” and “body systems charting.” No well-established, consistent, and standard practices, policies, or procedures related to conducting PA assessments were identified by participants.
Inpatient exercise spaces: Among participants who worked in inpatient settings, facilitators to nurses supporting patients to perform PA were identified. In particular, having an exercise room, the ability to put an exercise bike in a patient’s room, space to walk in hallways, and/or a recreation therapist who could meet with inpatients were cited as beneficial.
CFIR Outer Setting Domain: Oncology Nursing Profession at Large and External Oncology and Nursing Organizations
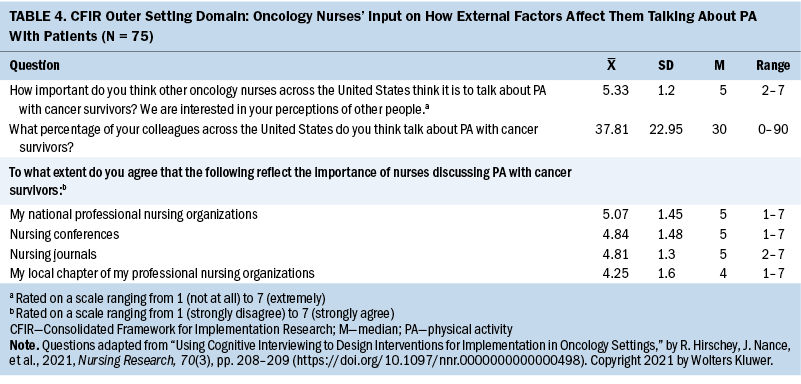
Quantitative data (see Table 4) revealed that participants believe that nationally, across the oncology nursing profession, few oncology nurses talk about PA with patients. When asked to rate their agreement that professional nursing organizations, conferences, and journals reflect the importance of promoting PA for patients on a scale ranging from 1 (strongly disagree) to 7 (strongly agree), the average rating among participants was 5. Participants’ responses to open-ended questions provided no additional insights into how the oncology nursing profession at large supports nurse recommendations of PA for patients.
Resources that meet patient needs: Participants identified a need for resources about PA that meet the needs of patients recovering from cancer treatments. For example, when referring to barriers to doing PA for patients who are hospitalized, one participant expressed the “need [for] options for patients who can’t leave [the] room often, like those on contact or enteric precautions.” Another participant expressed that they did not know about resources to support their patients after discharge “because they are very restricted in terms of going out in public, outside, to a gym, et cetera. There are a lot more barriers to exercise after discharge, and I’m not sure how to suggest they continue PA.” Among all participants, the need for additional patient PA resources was consistently noted.
CFIR Intervention Characteristics Domain: Nurses Providing PA Counseling
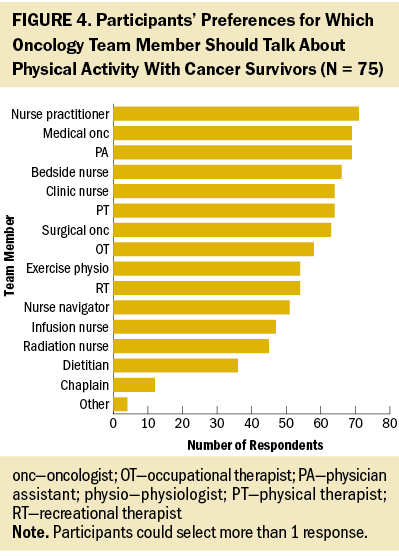
As detailed in Figure 4, quantitative data indicated that when oncology nurses were asked to identify all the people on the oncologic team who should talk about PA with patients, the nurse practitioner was the one role most often selected (n = 71), followed by the physician assistant and medical oncologist (n = 69 for both), the bedside nurse (n = 66), and the clinic nurse (n = 64).
The findings from the qualitative data offered several specific suggestions from oncology nurses about characteristics that should be incorporated in PA interventions. These specific suggestions relate to nurses’ perspectives about what will increase the feasibility and adaptability of PA interventions, as well as their ability to deliver such interventions.
Feasibility and adaptability: Participants provided a wide range of suggestions that would make PA counseling feasible in their clinical setting, indicating a need for interventions that are adaptable to the specific circumstances of a given clinical setting. For example, one participant suggested that a physician initiate the first conversation; other members of the interprofessional team would then reinforce the message, particularly nurses because they have the most contact with patients. Participants also indicated that they thought interventions should begin with discussions about the importance of PA at diagnosis—and before, if possible, in a preventive capacity—and continue throughout survivorship visits. Last, participants identified several specific materials that could be incorporated into interventions to promote oncology nurses’ discussion of PA with patients, including “resources that show patients what to do,” “monthly support groups,” “virtual visits (video and phone),” “community forums,” “newsletters to patients,” “podcasts,” “handouts,” “websites,” and “referrals to exercise therapy programs.” Among all participants, there was enthusiasm for support in discussing PA with patients.
Evidence-based guidance: Participants indicated that nursing education about the evidence supporting PA guidelines for cancer survivors is needed, particularly regarding safety considerations. For example, one participant indicated that receiving guidance on “best practices on timing for discussing PA and resources for safe PA for different diagnoses would be ideal.” Another participant said that they would like to receive “education for all levels (e.g., repositioning in a chair to prevent decline, muscles to promote [getting] on and off toilet)—functional movement is key—provided space and recommendations on consistent assessment and documentation.” One participant shared the following at the conclusion of the survey:
Even the act of completing this survey brought to my attention areas where I could and should expand my knowledge regarding how/when to encourage PA for patients. It is so important and should be standard discussion, not a low priority.
Across the board, participants noted a need for interventions that include nursing education about PA recommendations for individuals living beyond a cancer diagnosis.
Discussion
Collectively, the results from this study identified details about multilevel factors that can influence the design of a nurse-level PA intervention that will fit within the oncology clinic setting. Of note, these results represent the perspectives of oncology nurses, who lead the way in patient education and spend the most time with patients. In addition, patients may be particularly receptive to PA counseling from nurses because nurses are consistently rated as the most trusted profession in a U.S.-based poll (Saad, 2022). The nursing perspective is critical for interventionists to consider when designing future PA recommendations that are conducive to uptake and sustainability in clinical oncology settings.
The results indicated that oncology nurses have various beliefs about the appropriateness of recommending PA for patients, particularly those newly diagnosed with cancer. Reported concerns included being perceived as insensitive and burdening patients with instructions to do something that may be challenging during a difficult time. Yet, research shows that patients want guidance on PA during cancer treatment. For example, a cross-sectional study of 392 patients receiving outpatient cancer treatment reported that 80% of participants expressed interest in PA programs (Avancini et al., 2020). The American Cancer Society also recommends that PA counseling begin as soon as possible after a cancer diagnosis because it can significantly help patients prepare for and manage treatment and side effects, as well as improve long-term outcomes and quality of life (Rock et al., 2022). These findings point to the need for interventions that include nursing continuing education about the benefits of PA and the clinical importance of incorporating it into clinical oncology care.
The results also indicated that although oncology nurses believe it is important to discuss PA, they feel underprepared to do so. This finding is supported by the results from a qualitative study of 14 oncology nurses; the authors reported that education about PA for individuals living beyond a cancer diagnosis is necessary for nurses to encourage PA for this population (Avancini et al., 2021). Nurses’ feelings that they are underprepared to speak about PA recommendations and the necessary precautions to address for different patients may contribute to another of the current study’s findings—nurses feeling that they do not have enough time to discuss PA. It is reasonable that a lack of confidence surrounding PA recommendations may cause nurses to overestimate the amount of time needed to address PA.
Finally, the results indicate that oncology nurses need resources to support them in providing PA education to patients. Professional organizations have created clinician resources including ONS’s (n.d.) Get Up, Get Moving and ACSM’s (n.d.) Moving Through Cancer campaigns. In addition, nursing journals have published recommendations on how to incorporate considerations of the social determinants of health into PA counseling (Hirschey, Tan, et al., 2021), and the Oncology Nursing Podcast has discussed this topic (Hirschey & Jardine, 2022). A study by Forner et al. (2021) demonstrated that nurse PA coaching guided by ONS’s Get Up, Get Moving campaign, delivered in an infusion center and via telephone, positively influenced PA among individuals receiving chemotherapy and/or radiation therapy for breast, colon, or prostate cancers. Another nurse-led PA counseling intervention improved pain and quality of life among patients newly diagnosed with head and neck cancer (Hong et al., 2022). PA guidelines and resources put forth by national organizations can be used in nurse-led interventions to promote PA among patients.
Limitations
This research is not without limitations. First, most of the study participants met national PA recommendations themselves. Thus, it is reasonable that they had more favorable attitudes toward PA and were likely to discuss PA with patients because they were personally familiar with the general benefits. It is possible that the broader oncology nursing population is in even greater need of education about the importance of PA as part of cancer and survivorship treatment. Effective interventions may need to engage oncology nurses in PA so that they may become personally more favorable to and knowledgeable about it.
Second, data were collected in 2020 during the COVID-19 pandemic, which may have had a multitude of implications. Because of the pandemic, the healthcare workforce and nurses in particular have become more overworked and may have even less time to consider PA for patients. Therefore, the importance of providing resources and using a variety of intervention formats, such as those that are based on distance and supported by technology, may be even more important.
Finally, the results are solely from nurses’ perspectives. Perspectives from other members of the oncology care team and patients may also inform the design of PA interventions for implementation in clinical oncology settings. However, given that nurses are the people on the interprofessional care team who spend the most time with patients and provide the most patient education, these results are valuable and represent an important first step for improving delivery of PA recommendations to patients.
Implications for Research
The results from this study suggest that researchers designing PA interventions should consider how limited nursing time and training about PA will influence intervention implementation and sustainability beyond a research study period. Such approaches will lead to effective interventions that are feasible beyond research settings that provide extra resources and support for PA intervention delivery. Future research may focus on developing PA interventions for clinical settings that consider organizational readiness for change and perspectives from other members of the clinical care team. The results may also be applied to inform quality improvement efforts in which nurses may focus on setting-specific circumstances to lead PA promotion efforts specific to their practice.
Implications for Practice
Although this study focused on using implementation science approaches to inform the design of sustainable interventions, the results are relevant for current oncology nursing practice. Oncology nurses can seek continuing education about PA, become familiar with available evidence-based resources from ONS and ACSM, and work within their settings to implement PA-focused quality improvement projects. In addition, it is critical that clinical settings are adaptive to the relative priorities of tasks that nurses must consider during a given patient interaction. It is reasonable for nurses to provide brief education-based interventions. The success of such education is likely to depend on additional support from cancer centers, which may include resources and referrals to PA programs and professionals. In particular, providing PA education for non–English-speaking patients will require additional materials and translation services from cancer centers.
Conclusion
Patients living beyond a cancer diagnosis can benefit substantially from engaging in PA. Oncology nurses are poised to lead the way in improving the information that patients receive about the benefits of PA during and after cancer treatment. To support nurses in this important endeavor, researchers must design interventions that are responsive to the needs and circumstances in which oncology nurses may deliver such interventions. This study’s novel approach of designing interventions with the end point of clinical translation in mind holds promise for the development of a new wave of PA nursing interventions that are not only effective but also are implementable and sustainable in nursing practice.
About the Authors
Rachel Hirschey, PhD, RN, is an associate member in the Lineberger Comprehensive Cancer Center and an assistant professor in the School of Nursing; Mary Wangen, MPH, is a research associate in the Center for Health Promotion and Disease Prevention; Ayomide Okanlawon Bankole, PhD, RN, is a postdoctoral trainee in the School of Nursing; Becky Hoover, RN, BSN, is a doctoral candidate in the School of Nursing; Stephanie B. Wheeler, PhD, MPH, is the associate director of community outreach and engagement in the Lineberger Comprehensive Cancer Center and a professor in the Gillings School of Global Public Health; Jennifer Leeman, DrPH, MPH, MDiv, is a professor in the School of Nursing; and Ashley Leak Bryant, PhD, RN, OCN®, FAAN, is the assistant director of cancer research training education coordination in the Lineberger Comprehensive Cancer Center and an associate professor in the School of Nursing, all at the University of North Carolina at Chapel Hill. This research was funded, in part, by the National Institute on Minority Health and Health Disparities (K23 MD015719-01; principal investigator: Hirschey) and Sigma Theta Tau Alpha Alpha (principal investigator: Hirschey). Hirschey, Wangen, Wheeler, Leeman, and Leak Bryant contributed to the conceptualization and design. Hirschey completed the data collection and provided statistical support. Hirschey, Wangen, and Wheeler provided the analysis. All authors contributed to the manuscript preparation. Hirschey can be reached at hirschey@unc.edu, with copy to ONFEditor@ons.org. (Submitted September 2022. Accepted December 20, 2022.)
References
Alderman, G., Semple, S., Cesnik, R., & Toohey, K. (2020). Health care professionals’ knowledge and attitudes toward physical activity in cancer patients: A systematic review. Seminars in Oncology Nursing, 36(5), 151070. https://doi.org/10.1016/j.soncn.2020.151070
American College of Sports Medicine. (n.d.). Moving Through Cancer. https://www.exerciseismedicine.org/eim-in-action/moving-through-cancer
Avancini, A., D’Amico, F., Tregnago, D., Trestini, I., Belluomini, L., Vincenzi, S., . . . Pilotto, S. (2021). Nurses’ perspectives on physical activity promotion in cancer patients: A qualitative research. European Journal of Oncology Nursing, 55, 102061. https://doi.org/10.1016/j.ejon.2021.102061
Avancini, A., Pala, V., Trestini, I., Tregnago, D., Mariani, L., Sieri, S., . . . Lanza, M. (2020). Exercise levels and preferences in cancer patients: A cross-sectional study. International Journal of Environmental Research and Public Health, 17(15), 5351. https://doi.org/10.3390/ijerph17155351
Bernardo, L.M., & Becker, B.J. (Eds.). (2016). Integrating physical activity into cancer care: An evidence-based approach. Oncology Nursing Society.
Breimaier, H.E., Heckemann, B., Halfens, R.J.G., & Lohrmann, C. (2015). The Consolidated Framework for Implementation Research (CFIR): A useful theoretical framework for guiding and evaluating a guideline implementation process in a hospital-based nursing practice. BMC Nursing, 14, 43. https://doi.org/10.1186/s12912-015-0088-4
Campbell, K.L., Winters-Stone, K.M., Wiskemann, J., May, A.M., Schwartz, A.L., Courneya, K.S., . . . Schmitz, K.H. (2019). Exercise guidelines for cancer survivors: Consensus statement from International Multidisciplinary Roundtable. Medicine and Science in Sports and Exercise, 51(11), 2375–2390. https://doi.org/10.1249/MSS.0000000000002116
Cantwell, M., Walsh, D., Furlong, B., Moyna, N., McCaffrey, N., Boran, L., . . . Woods, C. (2018). Healthcare professionals’ knowledge and practice of physical activity promotion in cancer care: Challenges and solutions. European Journal of Cancer Care, 27(2), e12795. https://doi.org/10.1111/ecc.12795
Cohn, D., Brown, A., & Lopez, M.H. (2021, May 14). Black and Hispanic Americans see their origin as central to who they are, less so for White adults. Pew Research Center. https://www.pewresearch.org/social-trends/2021/05/14/black-and-hispanic…
Damschroder, L.J., Aron, D.C., Keith, R.E., Kirsh, S.R., Alexander, J.A., & Lowery, J.C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50. https://doi.org/10.1186/1748-5908-4-50
Damschroder, L.J., Reardon, C.M., Widerquist, M.A.O., & Lowery, J.C. (2022). The updated Consolidated Framework for Implementation Research based on user feedback. Implementation Science, 17, 75. https://doi.org/10.1186/s13012-022-01245-0
Forner, J.K., Doughty, A., Dalstrom, M., Messer, B.L., & Lizer, S.K. (2021). Quality of life: A nurse-led physical activity coaching program to improve the quality of life of patients with cancer during the COVID-19 pandemic. Clinical Journal of Oncology Nursing, 25(5), 571–577. https://doi.org/10.1188/21.CJON.571-577
Gonzalez-Hermoso, J., & Santos, R. (2019, October 15). Separating race from ethnicity in surveys risks an inaccurate picture of the Latinx community. Urban Institute. https://www.urban.org/urban-wire/separating-race-ethnicity-surveys-risk…
Hardcastle, S.J., Kane, R., Chivers, P., Hince, D., Dean, A., Higgs, D., & Cohen, P.A. (2018). Knowledge, attitudes, and practice of oncologists and oncology health care providers in promoting physical activity to cancer survivors: An international survey. Supportive Care in Cancer, 26(11), 3711–3719. https://doi.org/10.1007/s00520-018-4230-1
Harris, P.A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., & Conde, J.G. (2009). Research Electronic Data Capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Hirschey, R., & Jardine, S. (Hosts). (2022, February 18). Exercise’s effect on patient and provider well-being (No. 195) [Audio podcast episode]. In Oncology Nursing Podcast. Oncology Nursing Society. https://www.ons.org/podcasts/episode-195-exercises-effect-patient-and-p…
Hirschey, R., Nance, J., Wangen, M., Bryant, A.L., Wheeler, S.B., Herrera, J., & Leeman, J. (2021). Using cognitive interviewing to design interventions for implementation in oncology settings. Nursing Research, 70(3), 206–214. https://doi.org/10.1097/NNR.0000000000000498
Hirschey, R., Tan, K., Petermann, V.M., & Leak Bryant, A. (2021). Healthy lifestyle behaviors: Nursing considerations for social determinants of health. Clinical Journal of Oncology Nursing, 25(5, Suppl.), 42–48. https://doi.org/10.1188/21.CJON.S1.42-48
Hong, Y.-L., Hsieh, T.-C., Chen, P.-R., & Chang, S.-C. (2022). Nurse-led counseling intervention of postoperative home-based exercise training improves shoulder pain, shoulder disability, and quality of life in newly diagnosed head and neck cancer patients. Journal of Clinical Medicine, 11(14), 4032. https://doi.org/10.3390/jcm11144032
Hsieh, H.-F., & Shannon, S.E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687
Jones, L.W., & Alfano, C.M. (2013). Exercise–oncology research: Past, present, and future. Acta Oncologica, 52(2), 195–215. https://doi.org/10.3109/0284186X.2012.742564
Keogh, J.W., Pühringer, P., Olsen, A., Sargeant, S., Jones, L.M., & Climstein, M. (2017). Physical activity promotion, beliefs, and barriers among Australasian oncology nurses. Oncology Nursing Forum, 44(2), 235–245. https://doi.org/10.1188/17.ONF.235-245
Leeman, J., Baquero, B., Bender, M., Choy-Brown, M., Ko, L.K., Nilsen, P., . . . Birken, S.A. (2019). Advancing the use of organization theory in implementation science. Preventive Medicine, 129S, 105832. https://doi.org/10.1016/j.ypmed.2019.105832
MacVicar, M.G., Winningham, M.L., & Nickel, J.L. (1989). Effects of aerobic interval training on cancer patients’ functional capacity. Nursing Research, 38(6), 348–351.
Nadler, M., Bainbridge, D., Tomasone, J., Cheifetz, O., Juergens, R.A., & Sussman, J. (2017). Oncology care provider perspectives on exercise promotion in people with cancer: An examination of knowledge, practices, barriers, and facilitators. Supportive Care in Cancer, 25(7), 2297–2304. https://doi.org/10.1007/s00520-017-3640-9
National Institutes of Health. (2016). Dissemination and implementation research in health (R01). U.S. Department of Health and Human Services. https://grants.nih.gov/grants/guide/pa-files/par-16-238.html
Oncology Nursing Society. (n.d.). Get Up, Get Moving. https://www.ons.org/make-a-difference/quality-improvement/get-up-get-mo…
Parker, K., Horowitz, J.M., Morin, R., & Lopez, M.H. (2015, June 11). Chapter 7: The many dimensions of Hispanic racial identity. Pew Research Center. https://www.pewresearch.org/social-trends/2015/06/11/chapter-7-the-many…
Patel, A.V., Friedenreich, C.M., Moore, S.C., Hayes, S.C., Silver, J.K., Campbell, K.L., . . . Matthews, C.E. (2019). American College of Sports Medicine Roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Medicine and Science in Sports and Exercise, 51(11), 2391–2402. https://doi.org/10.1249/MSS.0000000000002117
Prip, A., Møller, K.A., Nielsen, D.L., Jarden, M., Olsen, M.-H., & Danielsen, A.K. (2018). The patient–healthcare professional relationship and communication in the oncology outpatient setting: A systematic review. Cancer Nursing, 41(5), E11–E22. https://doi.org/10.1097/NCC.0000000000000533
Rock, C.L., Thomson, C.A., Sullivan, K.R., Howe, C.L., Kushi, L.H., Caan, B.J., . . . McCullough, M.L. (2022). American Cancer Society nutrition and physical activity guideline for cancer survivors. CA: A Cancer Journal for Clinicians, 72(3), 230–262. https://doi.org/10.3322/caac.21719
Saad, L. (2022, January 12). Military brass, judges among profession at new image lows. Gallup. https://news.gallup.com/poll/388649/military-brass-judges-among-profess…
Schmitz, K.H., Campbell, A.M., Stuiver, M.M., Pinto, B.M., Schwartz, A.L., Morris, G.S., . . . Matthews, C.E. (2019). Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA: A Cancer Journal for Clinicians, 69(6), 468–484. https://doi.org/10.3322/caac.21579
Turner, R.R., Steed, L., Quirk, H., Greasley, R.U., Saxton, J.M., Taylor, S.J., . . . Bourke, L. (2018). Interventions for promoting habitual exercise in people living with and beyond cancer. Cochrane Database of Systematic Reviews, 9(9), CD010192. https://doi.org/10.1002/14651858.CD010192.pub3
Von Ah, D., Brown, C.G., Brown, S.J., Bryant, A.L., Davies, M., Dodd, M., . . . Cooley, M.E. (2019). Research Agenda of the Oncology Nursing Society: 2019–2022. Oncology Nursing Forum, 46(6), 654–669. https://doi.org/10.1188/19.ONF.654-669
Winningham, M.L., & MacVicar, M.G. (1988). The effect of aerobic exercise on patient reports of nausea. Oncology Nursing Forum, 15(4), 447–450.
Winningham, M.L., MacVicar, M.G., Bondoc, M., Anderson, J.I., & Minton, J.P. (1989). Effect of aerobic exercise on body weight and composition in patients with breast cancer on adjuvant chemotherapy. Oncology Nursing Forum, 16(5), 683–689.
Wong, J.N., McAuley, E., & Trinh, L. (2018). Physical activity programming and counseling preferences among cancer survivors: A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 15(1), 48. https://doi.org/10.1186/s12966-018-0680-6
Younas, A., & Porr, C. (2018). A step-by-step approach to developing scales for survey research. Nurse Researcher, 26(3), 14–19. https://doi.org/10.7748/nr.2018.e1585




