Patient-Reported Measures of a Breast Cancer Nurse Navigator Program in an Underserved, Rural, and Economically Disadvantaged Patient Population
Objectives: To assess the efficacy of the University of New Mexico Comprehensive Cancer Center’s (UNMCCC’s) breast cancer nurse navigator (BCNN) program in addressing gaps in cancer care for an underserved, rural, and economically disadvantaged population.
Sample & Setting: 54 navigated patients under the care of the BCNN and 32 non-navigated patients whose care began prior to the start of the program.
Methods & Variables: Surveys were administered anonymously to patients during regularly scheduled appointments at UNMCCC.
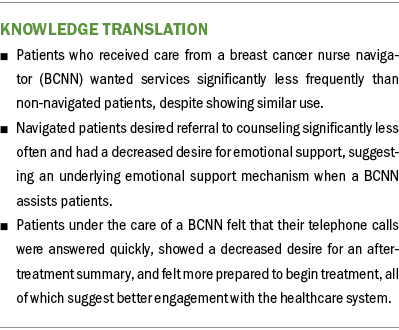
Results: Navigated patients more strongly agreed that they were prepared for the beginning of treatment and that calls were returned promptly, and showed a decreased desire for an after-treatment summary compared to non-navigated patients.
Implications for Nursing: Navigated patients report better understanding of and engagement with the healthcare system when assisted by a BCNN during breast cancer treatment with curative intent, as well as desire fewer services than non-navigated peers, indicating greater satisfaction.
Jump to a section
Nurse navigators are designated nurses who are specially trained to follow and support patients and families through cancer treatment (Freeman, 2012). One of the goals of a nurse navigator is to ensure that patients, particularly those with lower socioeconomic status, can move effectively through the system and receive the best care possible in a timely manner. Many programs designed to reduce racial and ethnic disparities in breast cancer care use nurse navigators to further that goal (Capitman et al., 2019; Freeman, 2006a, 2006b; Freeman et al., 1995).
The University of New Mexico Comprehensive Cancer Center’s (UNMCCC’s) patient population is socioeconomically diverse, with a population that is highly rural, of lower socioeconomic status, and largely comprised of people of color. In the 2020 census, New Mexico’s population was 47.7% Hispanic, which was the highest percentage in the nation, and 8.9% Native American, second only to Alaska. The population was also 21% rural, a significantly higher percentage than in other southwestern states (U.S. Census Bureau, 2021a). UNMCCC’s catchment area is the entire state of New Mexico, which measures 121,000 square miles and is the fifth largest and sixth least densely populated state in the United States (U.S. Census Bureau, 2021b). Were one to overlay the land mass of New Mexico over the Eastern Seaboard, half of it would include 20 National Cancer Institute–designated cancer centers (UNMCCC, n.d.).
People of color and rural patients face disadvantages in many areas of health, and breast cancer is no different. Although Hispanic women—a large population at UNMCCC—are less likely to develop breast cancer than non-Hispanic White women, they are more likely to be diagnosed at the regional stage rather than at the localized stage (Banegas & Li, 2012; Power et al., 2018). This trend of late diagnosis of breast cancer may also be true for some Native American women (Kaur et al., 2014). For example, despite an overall decrease in mortality from breast cancer in the U.S. general population, the rate for Native American women remained broadly flat from 1990 to 2009 (White et al., 2014). These disadvantages are also similar to the well-studied disparities faced by Black breast cancer survivors (Husain et al., 2019). Regarding socioeconomic status, New Mexico has the lowest percentage of employer-provided insurance coverage (36.6%) and the highest percentage of Medicaid coverage (32.7%) of the 50 states, excluding data from Puerto Rico. New Mexico is also one of only six states where more than half of births are financed by Medicaid (54%) (Gifford et al., 2017; Kaiser Family Foundation, 2019).
Previous studies have found that in highly coordinated healthcare systems like UNMCCC—where providers, imaging services, and ancillary services are co-located—navigated patients receive significantly better care coordination, psychosocial care, and patient education than their non-navigated peers (Campbell et al., 2010; Wagner et al., 2014). In addition, patients who are navigated may experience a reduction in the time between diagnosis and start of treatment (Rohsig et al., 2019), although applicability to the current study’s patient population and care setting is limited. The effect of navigation on patient understanding seems to be reproducible, as 90% of those who received information from a breast cancer nurse navigator (BCNN) felt satisfied and comfortable with their understanding of the disease (Trevillion et al., 2015). Similarly, prior research has shown that patient satisfaction is higher and distress is lower in navigated patients than in non-navigated patients (Dillon et al., 2021; Williams et al., 2004). According to Mertz et al. (2017), 42% of Australian people with breast cancer agreed that having a navigator-like contact would have improved their care experience. Many studies have attempted to measure the cost of healthcare usage with a BCNN, with some showing no difference in expenditure between navigated and non-navigated patients with breast cancer and others showing a significant increase after a telemedicine nurse navigator consult (Adler et al., 2019; Mertz et al., 2017). None have assessed whether a difference exists in patients’ desires for service usage.
With the goal of improving care coordination, psychosocial care, patient education, and healthcare usage, UNMCCC instituted a BCNN program in 2017 to help guide patients within the organization. UNMCCC currently employs one full-time BCNN specifically for patients with breast cancer undergoing treatment with curative intent. This study aimed to evaluate usage of the BCNN program at UNMCCC by comparing the desire for services, use of services, and feelings of preparedness between navigated and non-navigated patients.
Methods
Sample and Setting
Surveys to assess patient satisfaction and services used were administered anonymously during regularly scheduled appointments at UNMCCC between April 29 and June 7, 2019, to patients with breast cancer who were either undergoing or had previously undergone treatment with curative intent. The survey was designed by the authors, with input from other stakeholders in the BCNN program at UNMCCC, including oncologists and the BCNN. This study was reviewed by the University of New Mexico Institutional Review Board, and consent was deemed not necessary because of the de-identified nature of the data collection.
Procedures and Data Analyses
Patients under the care of the BCNN (navigated patients) and those whose care began prior to the beginning of the program (non-navigated patients) were assessed. Patients were assessed at any point after completion of definitive treatment (surgery, chemotherapy, radiation therapy, or a combination thereof), but may have been receiving adjuvant endocrine therapy at the time that the surveys were completed. All patients with regularly scheduled appointments meeting the eligibility criteria were noted by the BCNN, clinic nurses, and physicians. Surveys were then administered to patients by the medical assistant who performed check-in and rooming of all patients. Patients were instructed to leave their completed survey in the room. The medical assistant collected the completed surveys while preparing the room for the next patient and placed them in a secure box in the nursing station. Surveys that were incomplete or not completed were securely discarded.
Overall, 32 non-navigated patients and 54 navigated patients completed the survey. Baseline patient demographics and questions regarding patients’ specific point in their treatment journey were omitted in the hopes of shortening the survey and increasing the response rate, while also protecting patient confidentiality. The survey was written in English, but interpretation services were available from an in-person Spanish interpreter if needed. The first section of the survey focused on patients’ experiences with the BCNN or office staff, such as whether they felt adequately prepared to start treatment, whether telephone calls were returned quickly, and how well patients perceived side effects to be controlled. Patients were asked to circle the degree to which they agreed with each statement on a Likert-type scale, and each response option was converted to a numeric score ranging from 1 to 5 (1 = strongly agree, 2 = agree, 3 = neutral, 4 = disagree, and 5 = strongly disagree). A Likert-type scale was used to standardize responses and allow for statistical comparison of highly subjective statements. For navigated patients, the statements referred to the BCNN as the source of support, whereas for non-navigated patients, “nurse navigator” was replaced with “office staff.” The definition of “office staff” was left intentionally vague because patients interact with many different roles throughout treatment at UNMCCC, and the intent was to ensure that all staff were included. Physicians and advanced practice providers were intentionally and explicitly omitted.
The second group of questions was related to service usage and the desire for services. The instructions asked patients to rank the importance of their usage of or desire for use of services, such as educational information, appointment scheduling, emotional support, transportation assistance, and referral for financial and insurance assistance, on a scale from 1 to 9, with 1 being the most important, 2 being the second most important, and so on. However, only seven patients between both groups used the scale as intended. Instead, most patients ranked the items based on value (i.e., 9s on three items and 1s on two items, with the remainder left blank). This complicated the analysis of these data significantly, and, as such, two different analyses were performed. The first analysis was conducted based on the small number of patients who answered the questions as intended, which used the values as recorded by the patients. For the second analysis, which was intended to ensure that all responses were counted, responses were converted into binary responses, with any response counting as 1 and no response counting as 0. For both the ranked and binary analyses, results from each category, the desire for further services, and the strength of their importance to patients were summed to get an overall measurement of use of services.
For the intended Likert-type scale response analysis and the binary response analysis, statistical analyses included t tests with two tails and 95% confidence intervals. Analyses assumed unequal variation between groups because of the different numbers of responses in each group and an alpha of 0.05.
Results
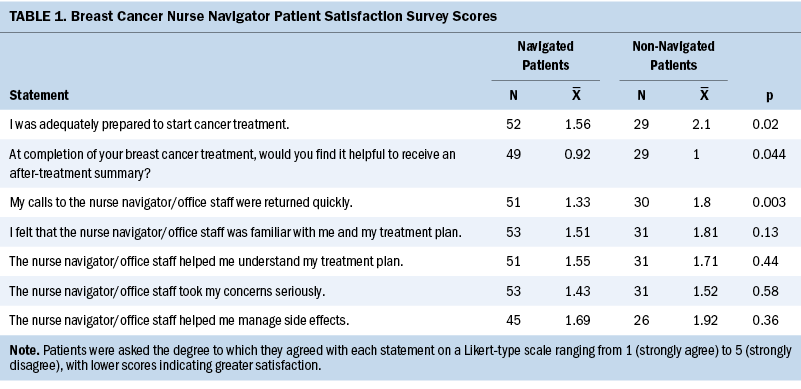
From April to May 2020, a total of 86 patients completed the surveys (n = 54 navigated patients and n = 32 non-navigated patients). Navigated patients more strongly agreed that they were prepared for the beginning of treatment as compared to non-navigated patients (mean = 1.56 versus mean = 2.1, p = 0.02) (see Table 1). Navigated patients also showed a decreased desire for an after-treatment summary (mean = 0.92 versus mean = 1, p = 0.044), and they more strongly felt that their calls were returned promptly when compared to non-navigated patients (mean = 1.33 versus mean = 1.8, p = 0.003). Navigated patients were more likely to agree that the BCNN was more knowledgeable about their treatment plan (mean = 1.51 versus mean = 1.81, p = 0.13), better helped them to understand their treatment plans (mean = 1.55 versus mean = 1.71, p = 0.44), took their concerns more seriously (mean = 1.43 versus mean = 1.52, p = 0.58), and better helped them to manage side effects (mean = 1.69 versus mean = 1.92, p = 0.36) as compared to office staff for non-navigated patients, but these results were not statistically significant.
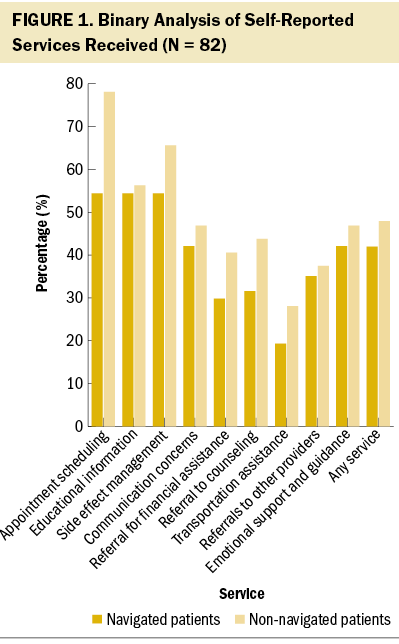
There was no statistically significant difference in use of any service except for appointment scheduling, with navigated patients using scheduling services at a significantly lower rate than non-navigated patients (54% versus 78%, p = 0.017) (see Figure 1). Compared to non-navigated patients, there was a non–statistically significant decrease in use of educational information (54% versus 56%, p = 0.92), assistance with side effect management (54% versus 66%, p = 0.59), help with communication concerns (42% versus 47%, p = 0.83), referral for financial and insurance assistance (30% versus 41%, p = 0.4), referral to counseling (32% versus 44%, p = 0.724), referral for transportation assistance (19% versus 28%, p = 0.457), assistance with referrals to other providers (35% versus 38%, p = 0.97), and emotional support and guidance (42% versus 47%, p = 0.83) among navigated patients. There was not a significant difference when aggregating all services together, with 42% of navigated patients and 48% of non-navigated patients using the services measured (p = 0.11).
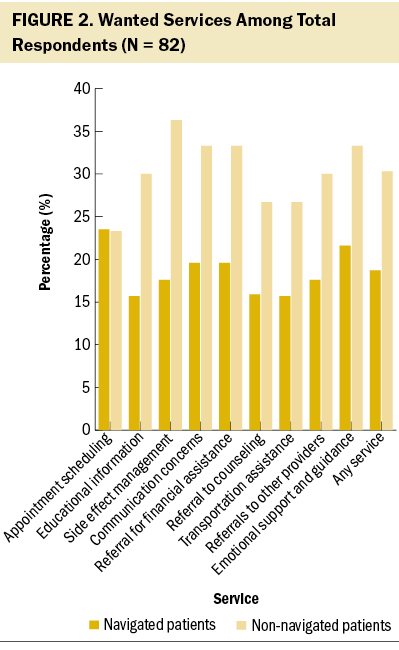
Overall, navigated patients wanted services significantly less than non-navigated patients (19% versus 30%, p = 0.00017), and navigated patients desired referral to counseling significantly less often (16% versus 27%, p = 0.048) (see Figure 2). There was also subjectively less desire for educational information (16% versus 30%, p = 0.24), assistance with side effect management (18% versus 36%, p = 0.097), assistance with communication concerns (20% versus 33%, p = 0.17), referral for financial and insurance assistance (20% versus 33%, p = 0.19), referral for transportation assistance (16% versus 27%, p = 0.26), assistance with referrals to other providers (18% versus 30%, p = 0.23), and emotional support and guidance (22% versus 33%, p = 0.22), but these differences were not significant. There was no difference in desire for help with appointment scheduling (24% versus 23%, p = 0.98).
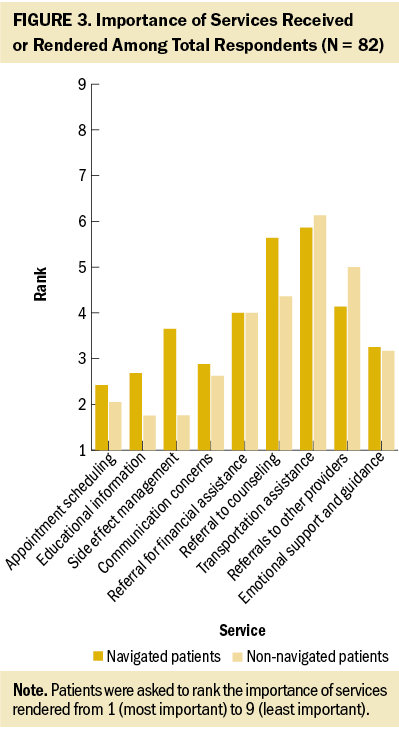
When patients were asked to rank the importance of services rendered by the BCNN or the office staff, navigated patients were less likely to rank most services as very important, including assistance with appointment scheduling (mean = 2.42 versus mean = 2.05, p = 0.39), assistance with communication concerns (mean = 2.88 versus mean = 2.62, p = 0.41), referral to counseling and support groups (mean = 5.64 versus mean = 4.36, p = 0.34), assistance with the management of symptoms and side effects (mean = 3.65 versus mean = 1.76, p = 0.41), and educational information (mean = 2.68 versus mean = 1.75, p = 0.054) (see Figure 3). There was no difference between groups in ranking the importance of emotional support and guidance (mean = 3.25 versus mean = 3.17, p = 0.93), assistance with transportation (mean = 5.86 versus mean = 6.13, p = 0.88), and referrals for financial assistance (mean = 4 for both groups, p = 1). With all data points combined, navigated patients ranked services used as slightly less important to them than non-navigated patients (mean = 3.34 versus mean = 3.09, p = 0.21), without a statistically significant difference.
When measuring the number of patients with a primary care provider, 50 navigated patients and 29 non-navigated patients reported having a primary care provider (p = 0.53).
Discussion
Patients under the care of the BCNN wanted services significantly less frequently than their non-navigated peers while showing similar use, suggesting that navigated patients were able to access all the services they wanted through the BCNN. These results support prior research from the United States and other countries that found that patients reported overall higher satisfaction with care received and increased feelings of control over their care when under the care of a BCNN (Berezowska et al., 2021; Dillon et al., 2021; Hook et al., 2012; Loiselle et al., 2020; Mertz et al., 2017).
Further supporting the belief that navigated patients are more satisfied with the care they received was the stronger agreement that they were prepared for the beginning of treatment (1.56 versus 2.1, p = 0.02) and the perception that their telephone calls were returned more quickly (1.33 versus 1.8, p = 0.003), all while showing a decreased desire for an after-treatment summary (0.92 versus 1, p = 0.044). Considering the retrospective nature of the survey questions, the study results also indicate that patients under the care of a BCNN felt more knowledgeable overall about their care, which supports the findings of a previous study in a similar system (Wagner et al., 2014). Patients’ satisfaction and feelings of control, combined with the decrease in use of services, are similar to the findings of a randomized controlled trial conducted in the Netherlands (Berezowska et al., 2021), which has a healthcare system with significantly different barriers to care and a very different patient population.
The decrease in use of assistance with scheduling appointments between patients receiving care from the BCNN and patients receiving care from office staff (54% versus 78%, p = 0.017) indicated that the BCNN acted prior to the patient needing intervention. This supports previous research showing that the use of a BCNN decreased the time between diagnosis and treatment by scheduling appointments more quickly, which may have led to meaningful differences in outcomes, particularly for patients of lower socioeconomic status and underrepresented patients, who often experience delays in care (Battaglia et al., 2007; Husain et al., 2019). The BCNN may have also served as a proxy for other services, such as psychiatric care and nutrition, by counseling patients, thereby eliminating the desire for formal consultation with these services. Navigated patients desired referral to counseling significantly less often than non-navigated patients (16% versus 27%, p = 0.048) which, in conjunction with the subjective decrease in desire for emotional support (22% versus 33%, p = 0.22), suggests that there is an underlying emotional support mechanism when a BCNN assists patients. This is an area shown to be of significant importance to women aged younger than 50 years (Pedersen et al., 2014).
Limitations
This study has several limitations. Although the survey was conducted in a prospective manner, patients were asked to recall their past experience with cancer treatment after definitive therapy, which may introduce recall bias. The surveys were not validated either psychometrically or via a process for face validation in this population, potentially allowing bias to be introduced in the questions. This was a small study, which likely limited the power of the analysis to detect meaningful differences and may have limited the results. The different styles of responses to the ranking in the second section of the survey presented another challenge, further limiting the sample size and intended analysis, and possibly masking statistically significant effects. The instructions were likely the source of confusion, which asked patients to do the following: “Rank all those you thought were important, with 1 being the most important, 2 being the second most important, etc. You do not have to rank all options.” Further clarity, such as “Rank only one option as 1,” would have likely prevented this.
Nurse navigation programs vary broadly from system to system, reflecting local needs as intended, so the generalizability of this work may be limited (Paskett et al., 2011). The integrated nature of UNMCCC, where all oncology services outside of major surgical care and inpatient management are co-located in one building, could potentially show different results than would be seen in a more fragmented care system. However, in a more fragmented system, the effects of a BCNN may be even more pronounced. Lastly, treatments may change over time, practices can vary among oncology providers, and disease stage differs among patients. Therefore, it is unlikely that patients received the exact same care, resulting in both inter- and intragroup variations.
Implications for Nursing and Conclusion
The results of this study showed that patients in a diverse, underrepresented, rural, and economically disadvantaged population report better understanding of and engagement with the healthcare system when assisted by a BCNN during the treatment of breast cancer with curative intent. Patients who received care from a BCNN desired fewer services than their non-navigated peers, indicating greater overall satisfaction with their cancer care. Understanding of and engagement with health care, as well as patient satisfaction, are all important aspects of patient care, particularly because underserved populations are at increased risk of poor outcomes. Therefore, these areas merit future research to mitigate health disparities and ensure equitable care for all patients.
The authors gratefully acknowledge medical assistants Patricia Kuhne and Susan Martinez, without whom patients would not have received the study surveys.
About the Authors
Michael A. Williams, MD, is a resident physician in the Department of Internal Medicine in the School of Medicine at the University of New Mexico; and Dianne R. Nielsen, RN, BSN, CNBN, CBCN, is a nurse navigator, Zoneddy Dayao, MD, is a medical oncologist, Ursa Brown-Glaberman, MD, is an associate professor, and Bernard Tawfik, MD, is an assistant professor, all in the Division of Internal Medicine in the Section of Hematology and Oncology at the University of New Mexico Comprehensive Cancer Center, all in Albuquerque. Brown-Glaberman has previously consulted for Biotheranostics; Seagen Inc., formerly known as Seattle Genetics; Taiho; and Sanofi. Williams and Dayao completed the data collection. Williams and Tawfik provided statistical support. Williams, Dayao, Brown-Glaberman, and Tawfik provided the analysis. Williams and Tawfik contributed to the manuscript preparation. All authors contributed to the conceptualization and design. Williams can be reached at miwilliams@salud.unm.edu, with copy to ONFEditor@ons.org. (Submitted July 2021. Accepted May 4, 2022.)
References
Adler, G., Kaufman, G., & Simon-Tuval, T. (2019). Healthcare utilization of breast cancer patients following telephone-based consultations of oncology nurse navigator via telemedical care. PLOS ONE, 14(5), e0216365. https://doi.org/10.1371/journal.pone.0216365
Banegas, M.P., & Li, C.I. (2012). Breast cancer characteristics and outcomes among Hispanic Black and Hispanic White women. Breast Cancer Research and Treatment, 134(3), 1297–1304. https://doi.org/10.1007/s10549-012-2142-1
Battaglia, T.A., Roloff, K., Posner, M.A., & Freund, K.M. (2007). Improving follow-up to abnormal breast cancer screening in an urban population: A patient navigation intervention. Cancer, 109(Suppl. 2), 359–367. https://doi.org/10.1002/cncr.22354
Berezowska, A., Passchier, E., & Bleiker, E. (2021). Professional patient navigation in a hospital setting: A randomized controlled trial. Supportive Care in Cancer, 29(4), 2111–2123. https://doi.org/10.1007/s00520-020-05721-5
Campbell, C., Craig, J., Eggert, J., & Bailey-Dorton, C. (2010). Implementing and measuring the impact of patient navigation at a comprehensive community cancer center. Oncology Nursing Forum, 37(1), 61–68. https://doi.org/10.1188/10.ONF.61-68
Capitman, J.A., Bhalotra, S., & Ruwe, M. (2019). Cancer and elders of color: Opportunities for reducing health disparities: Evidence review and recommendations for research and policy (1st ed.). Routledge. https://doi.org/10.4324/9781351162128
Dillon, E., Kim, P., Li, M., Huang, Q., Colocci, N., Cantril, C., & Hung, D. (2021). Breast cancer navigation: Using physician and patient surveys to explore nurse navigator program experiences. Clinical Journal of Oncology Nursing, 25(5), 579–586. https://doi.org/10.1188/21.CJON.579-586
Freeman, H.P. (2006a). Patient navigation: A community based strategy to reduce cancer disparities. Journal of Urban Health, 83(2), 139–141. https://doi.org/10.1007/s11524-006-9030-0
Freeman, H.P. (2006b). Patient navigation: A community centered approach to reducing cancer mortality. Journal of Cancer Education, 21(1, Suppl.), S11–S14. https://doi.org/10.1207/s15430154jce2101s_4
Freeman, H.P. (2012). The origin, evolution, and principles of patient navigation. Cancer Epidemiology, Biomarkers and Prevention, 21(10), 1614–1617. https://doi.org/10.1158/1055-9965.EPI-12-0982
Freeman, H.P., Muth, B.J., & Kerner, J.F. (1995). Expanding access to cancer screening and clinical follow-up among the medically underserved. Cancer Practice, 3(1), 19–30.
Gifford, K., Ellis, E., Coulter Edwards, B., Lashbrook, A., Hinton, E., Antonisse, L., . . . Rudowitz, R. (2017, October 19). Medicaid moving ahead in uncertain times: Results from a 50-state Medicaid budget survey for state fiscal years 2017 and 2018. Kaiser Family Foundation. https://www.kff.org/medicaid/report/medicaid-moving-ahead-in-uncertain-…
Hook, A., Ware, L., Siler, B., & Packard, A. (2012). Breast cancer navigation and patient satisfaction: Exploring a community-based patient navigation model in a rural setting. Oncology Nursing Forum, 39(4), 379–385. https://doi.org/10.1188/12.ONF.379-385
Husain, M., Nolan, T.S., Foy, K., Reinbolt, R., Grenade, C., & Lustberg, M. (2019). An overview of the unique challenges facing African-American breast cancer survivors. Supportive Care in Cancer, 27(3), 729–743. https://doi.org/10.1007/s00520-018-4545-y
Kaiser Family Foundation. (2019). Health insurance coverage of the total population. https://www.kff.org/other/state-indicator/total-population
Kaur, J.S., Vierkant, R.A., Hobday, T., & Visscher, D. (2014). Regional differences in breast cancer biomarkers in American Indian and Alaska Native women. Cancer Epidemiology, Biomarkers and Prevention, 23(3), 409–415. https://doi.org/10.1158/1055-9965.EPI-13-0738
Loiselle, C.G., Attieh, S., Cook, E., Tardif, L., Allard, M., Rousseau, C., . . . Talbot, D. (2020). The nurse pivot-navigator associated with more positive cancer care experiences and higher patient satisfaction. Canadian Oncology Nursing Journal, 30(1), 48–53. https://doi.org/10.5737/236880763014853
Mertz, B.G., Dunn-Henriksen, A.K., Kroman, N., Johansen, C., Andersen, K.G., Andersson, M., . . . Envold Bidstrup, P. (2017). The effects of individually tailored nurse navigation for patients with newly diagnosed breast cancer: A randomized pilot study. Acta Oncologica, 56(12), 1682–1689. https://doi.org/10.1080/0284186X.2017.1358462
Paskett, E.D., Harrop, J.P., & Wells, K.J. (2011). Patient navigation: An update on the state of the science. CA: A Cancer Journal for Clinicians, 61(4), 237–249. https://doi.org/10.3322/caac.20111
Pedersen, A.E., Hack, T.F., McClement, S.E., & Taylor-Brown, J. (2014). An exploration of the patient navigator role: Perspectives of younger women with breast cancer. Oncology Nursing Forum, 41(1), 77–88. https://doi.org/10.1188/14.ONF.77-88
Power, E.J., Chin, M.L., & Haq, M.M. (2018). Breast cancer incidence and risk reduction in the Hispanic population. Cureus, 10(2), e2235. https://doi.org/10.7759/cureus.2235
Rohsig, V., Silva, P., Teixeira, R., Lorenzini, E., Maestri, R., Saraiva, T., & Souza, A. (2019). Nurse navigation program: Outcomes from a breast cancer center in Brazil. Clinical Journal of Oncology Nursing, 23(1), E25–E31. https://doi.org/10.1188/19.CJON.E25-E31
Trevillion, K., Singh-Carlson, S., Wong, F., & Sherriff, C. (2015). An evaluation report of the nurse navigator services for the breast cancer support program. Canadian Oncology Nursing Journal, 25(4), 409–421. https://doi.org/10.5737/33688076254409414
University of New Mexico Comprehensive Cancer Center. (n.d.). National Cancer Institute designation. https://unmhealth.org/cancer/comprehensive/nci.html
U.S. Census Bureau. (2021a). Racial and ethnic diversity in the United States: 2010 census and 2020 census. https://www.census.gov/library/visualizations/interactive/racial-and-et…
U.S. Census Bureau. (2021b). 2020 census demographic data map viewer. https://www.census.gov/library/visualizations/2021/geo/demographicmapvi…
Wagner, E.H., Ludman, E.J., Aiello Bowles, E.J., Penfold, R., Reid, R.J., Rutter, C.M., . . . McCorkle, R. (2014). Nurse navigators in early cancer care: A randomized, controlled trial. Journal of Clinical Oncology, 32(1), 12–18. https://doi.org/10.1200/JCO.2013.51.7359
White, A., Richardson, L.C., Li, C., Ekwueme, D.U., & Kaur, J.S. (2014). Breast cancer mortality among American Indian and Alaska Native women, 1990–2009. American Journal of Public Health, 104(Suppl. 3), S432–S438. https://doi.org/10.2105/AJPH.2013.301720
Williams, P., Rankin, N., Redman, S., Davis, C., Armstrong, B., Malycha, P., & Girgis, A. (2004). National survey of women with early breast cancer: Their perceptions of care (1997). National Breast Cancer Centre. https://www.canceraustralia.gov.au/sites/default/files/publications/nsc…




